Births continue to fall in many Wyoming hospitals as lawmakers seek remedies for widening gaps in maternity care across the state.
Hospitals in Casper, Cheyenne, Rock Springs, Cody, Douglas and Lander are seeing declining deliveries, data from the Legislative Service Office shows. Four other hospitals — in Riverton, Kemmerer, Rawlins and most recently Evanston — have shut down birthing facilities entirely in recent years. When Evanston announced its closure at the end of 2024, it cited declining demand.
Wyoming’s maternity gap issue appears to be most acute in Central Wyoming, according to Curtis Biggs, Gov. Mark Gordon’s senior policy advisor, where SageWest Hospital in Lander is the main birthing facility serving a huge area of Fremont and Sublette counties.
“We are seeing a concerning trend of a decline in those births in that particular hospital, with a lot of births shifting to Thermopolis,” Biggs told the Legislature’s Joint Labor, Health & Social Services Committee Monday. The latter hospital was the only one presented that has experienced a significant spike in deliveries.
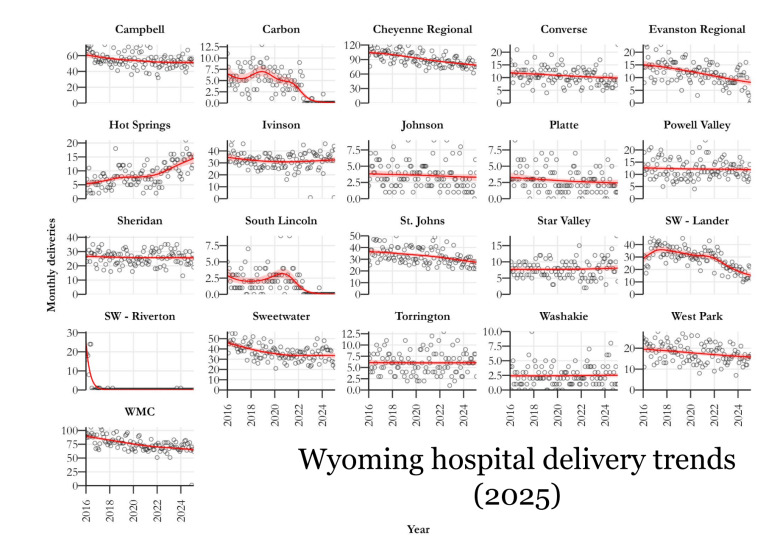 Births are declining in many Wyoming hospitals, these graphs show. (Wyoming Legislative Services Office)
Births are declining in many Wyoming hospitals, these graphs show. (Wyoming Legislative Services Office)
A dearth of maternal health care has made pregnancy and childbirth increasingly tricky in widening swaths of Wyoming, a 2023 WyoFile investigation found. This is evident in Fremont County, where moms are opting to temporarily relocate to places like Denver and even the East Coast to deliver babies. It is evident in Rawlins, where families have to travel Interstate 80, a notorious stretch of highway that closes frequently in the winter months, to deliver in Laramie. And it is evident in Teton County, where overflow patients from elsewhere in the state are straining providers.
Lawmakers made maternity care a top issue of study for the 2024 legislative off-season and began to identify a complicated mix of challenges for providing such care in rural places.
Maternity care is back on the table this summer as policymakers work to improve doctor recruitment, regulations and a complex system of health care reimbursements. Despite some steps forward in the past year, as Biggs explained to lawmakers, the options for families seeking robust maternal health care remain scant or nonexistent in many parts of the state.
The problem
A Wyoming Health Department assessment found that nearly half of the state’s counties lacked a practicing OB-GYN in 2024. The State Scorecard on Women’s Health and Reproductive Care ranked Wyoming 42nd that same year. The state placed behind all of its neighbors.
Solutions have been elusive. Complicating the issue are provider challenges like low birth volume in rural areas, high costs of medical malpractice insurance, financial viability struggles for hospitals, abortion ban impacts on doctors, liability concerns and barriers for midwives to deliver in hospitals.
Health care advocates have called on the state to expand Medicaid, promote midwifery and build partnerships that could boost care.
 Wyoming midwife Heidi Stearns checks an infant after a home birth. (Courtesy Teal Barmore Photography)
Wyoming midwife Heidi Stearns checks an infant after a home birth. (Courtesy Teal Barmore Photography)
Along with the 2024 legislative committee study, the OB Subcommittee of Gov. Gordon’s Health Task Force also worked to explore solutions. That group narrowed its focus last summer to three areas: how to better utilize midwives, doulas and family physicians alongside obstetricians in delivery care; the possibility of creating OB medical fellowships to bolster care in Wyoming; and regionalizing the state’s maternity care.
The Joint Labor Committee took up the issue once more as an interim topic in 2025. During its two-day meeting this week in Casper, Deputy Director of the Wyoming Department of Health Franz Fuchs and Gordon’s policy advisor Biggs laid out the situation anew.
“The primary problem we’re really diagnosing this with is hospital viability,” Fuchs said. “We believe that labor and delivery closures are really a symptom of broader financial stress on the hospitals, whether it’s due to low volume generally or management issues.”
That financial stress can come from a host of issues, he said, including low volume of births, management issues, nurse labor shortage and provider recruitment challenges, fewer women of childbearing age creating declining demand and comparatively low Medicaid payment rates. When stressed, hospitals look to offload services, he continued, and labor and delivery is an attractive candidate because it’s not profitable.
Fuchs offered several options for aiding hospitals, including increasing Medicaid hospital payment rates for deliveries, increasing Medicaid payments to delivering providers, increasing funding for provider recruitment programs and increasing provider education opportunities or incentives for medical students.
Other ideas that came up during the meeting were malpractice tort reform, mobile units that can travel to underserved areas and more oversight of the services local hospitals provide.
Steps and directions
Some steps have been taken to address the issue.
Blue Cross Blue Shield of Wyoming is launching a program in July to support maternal health and respond to growing concerns about access to care. The Maternity Care Program will include a subscription service for prenatal vitamins and remote monitoring for high-risk pregnancies or those living in areas with little or no maternity care, among other services.
Another step is a new OB residency track through the University of Wyoming Family Medicine Residency Program at Cheyenne.
“We have residents selected that will be on an OB track starting in July when they start their second year, which means our real goal is for them either then to be able to get into an OB fellowship following residency, or simply to go get a job, hopefully some place in the state,” said Dr. Jacques Beveridge, a Cheyenne OB-GYN.
He also echoed a common sentiment when he urged lawmakers’ “favorable consideration of increasing Medicaid payment.”
As vice president of the Wyoming Hospital Association, Josh Hannes served on the governor’s health task force OB subcommittee.
If the committee is not OK with the current state of maternity care, Hannes said, “and where we believe it’s going to go if there’s no intervention, and you believe that the state has a role to play in doing better, then I think there’s a number of valuable recommendations that have been presented that could take bill form. We would be supportive of those.”
Ultimately, committee members voiced support for pursuing bills that would: help give midwives more authority to deliver; raise Medicaid reimbursements for obstetrics; offer protections for pregnancy resource centers; look into mobile health units; and study other states’ models for helping to pay for malpractice insurance.
In addition, Rep. Rachel Rodriguez-Williams, R-Cody, who chairs the hard-right House Freedom Caucus, said she would like the health department to consider removing the COVID-19 vaccine from the list of recommended vaccines for pregnant women.
This article was originally published by WyoFile and is republished here with permission. WyoFile is an independent nonprofit news organization focused on Wyoming people, places and policy.
Related
