A mammography technician with a mammography machine. Public domain photo by National Cancer Institute
Early this summer, the U.S. Supreme Court ruled in the case of Kennedy v. Braidwood Management that a significant section of the Affordable Care Act was constitutional, meaning at least 100 million insured Americans are not required to pay out of pocket for initial preventive services.
The ruling on ACA Section 2713 requires most private insurers and Medicaid expansion programs to cover the cost of preventive services with A or B recommendations from the U.S. Preventive Services Preventive Task Force (USPSTF) with no cost-sharing (meaning no copayments, deductibles or co-insurance), as KFF explained at the time.
The June 27 SCOTUS ruling saves those 100 million Americans from having to pay out of pocket for initial preventive-screening tests. But many patients who have abnormalities on their initial free screening tests must pay substantial sums out of pocket for any needed tests and follow-up care.
“Reporters need to explain that we’ve fixed the problem now in two forms of cancer starting in January,” Fendrick commented. “They can let women know and other people assigned female at birth that they don’t have to worry about their deductibles or take out loans to get a diagnostic mammogram. They can get that done for no cost.”
“I hope journalists will report on the new policies for colorectal-, breast- and cervical-cancer screening and testing, and I hope their stories will increase initial screening and follow-up tests and ultimately save lives,” Fendrick wrote in an email.
Any woman needing a follow-up colonoscopy after getting a positive stool-sample test will get free follow-up screening tests, Fendrick said. But patients needing follow-up exams and patient navigation for colon-cancer screening will need to pay for those services, he added.
For some, a reprieve from high costs
Starting Jan. 1, patients who get an abnormal result during a screening mammogram for breast cancer will not need to pay for follow-up exams or patient navigation services under a new guideline from the federal Women’s Preventive Services Initiative (WPSI), said A. Mark Fendrick, M.D., an internal medicine physician and director of the Center for Value-Based Insurance Design at the University of Michigan.
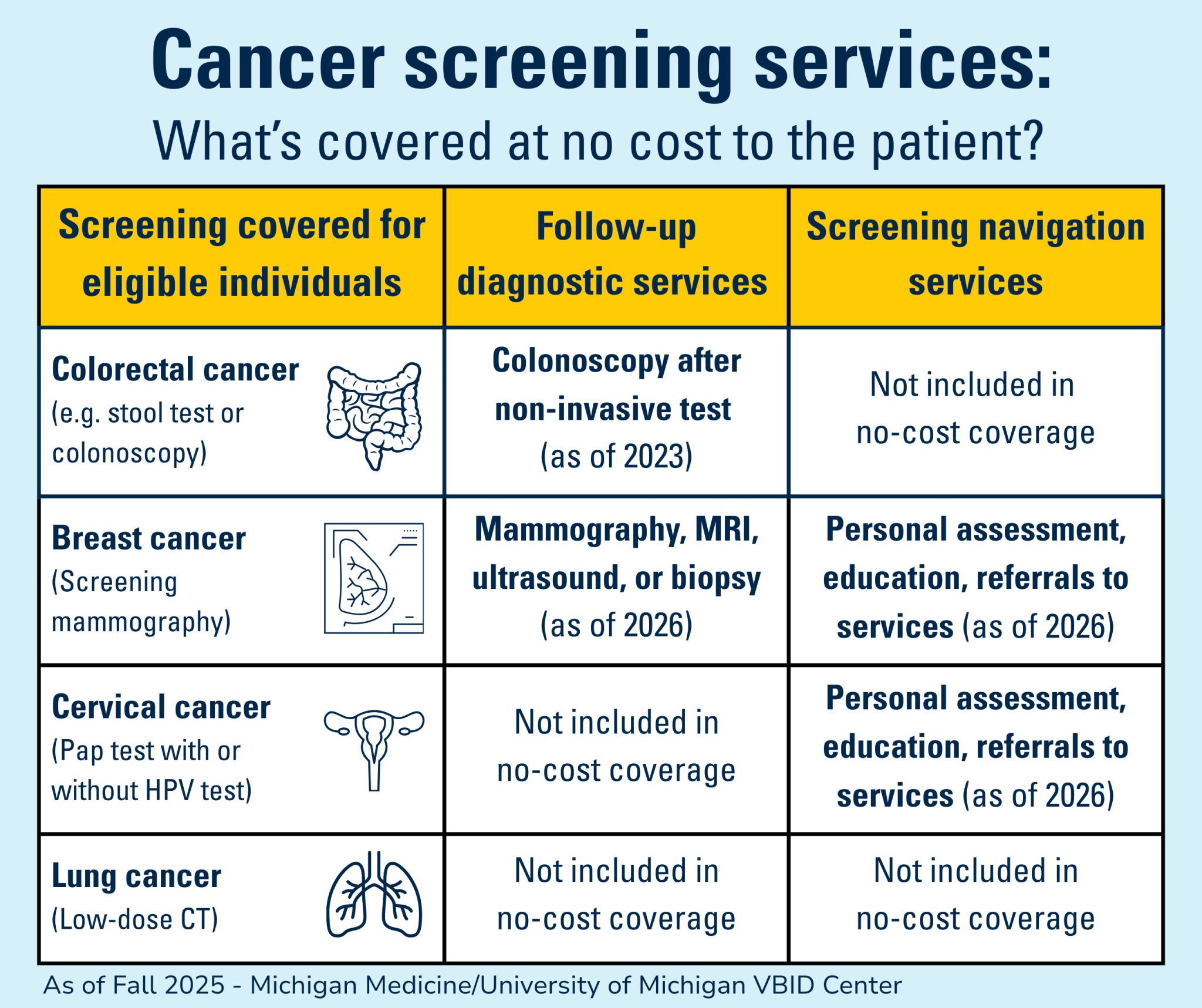
The same guideline applies to women who get cervical-cancer-screening tests showing a need for more tests. Those patients would get navigation services at no cost to them, but the guideline does not provide for no-cost follow-up tests, according to the August V-BID Center report.
Patient navigation involves educating patients on their need for additional tests and social services and any language or transportation barriers they need to overcome, the VBID report explained.
Since founding the VBID Center in 2005 with Michael Chernew, Ph.D., Fendrick has promoted policies to reduce patients’ out-of-pocket costs for essential clinical services such as vaccines and insulin. Also, the center advocated for the ACA preventive services provision that required coverage without cost sharing for initial screening for breast, cervical, colorectal and lung cancer. That provision did not explicitly specify coverage for needed follow-up tests or with no out-of-pocket costs, he said.
To date, Fendrick and colleagues have had limited success in three areas:
- Breast mammography. For patients who get an abnormal result after an initial mammography for breast-cancer, patients’ costs will be waived starting Jan. 1 for all follow-up testing and for navigation services. The rule applies to those with Medicaid and commercial insurance (such as ACA Marketplace coverage), Fendrick said.
- Cervical cancer screening. For women who get an abnormal initial screening result for cervical cancer, the WPSI guideline will waive patient costs for navigation (starting Jan. 1), but patients with Medicaid and commercial insurance will need to pay for follow-up diagnostic tests, Fendrick added.
- Colon cancer screening. For patients screened for colon cancer using an at-home stool-sample test, the VBID Center and other advocates argued successfully to eliminate cost sharing for follow-up diagnostic colonoscopies starting in 2023 for those with Medicare and commercial insurance, he explained, adding that insurers are not required to cover navigation services without cost sharing.
- Lung cancer screening. Health insurers can require cost sharing for follow-up tests and navigation for patients who get abnormal screening on an initial lung cancer screen.
Why this matters
Over the remainder of this year and into the next, journalists should report that beginning next year, insured patients screened for breast cancer should pay nothing for follow-up tests and navigation. “This is an important advancement versus the higher costs that patients screened for other cancers and other long-term conditions, such as HIV, will pay,” Fendrick commented.
“The purpose of cancer screening is to identify patients whose cancer can be prevented or detected early when treatments are usually more effective and less expensive,” Fendrick said in an email. “Given the prevalence of patients who have not followed up, it should not be difficult [for journalists] to identify them.”
Physicians and other providers who screen patients for early signs of cancer will know patients who do not return for more tests, Fendrick added. Also, reporters can call the American Cancer Society and individual cancer advocacy groups. “I have worked hard to put this on their radar,” he commented.
Many people do not get the recommended initial screening tests or follow-up exams because they don’t understand the need, have trouble finding the appropriate clinician and navigating the health system, Fendrick explained. Or, they may not be able to afford follow-up care, lack transportation or may need childcare, he added.
Cancer screening purgatory defined
Patients who get a free initial screening exam or test but then need further tests and navigation end up in what’s known informally as cancer-screening purgatory because they must pay for a follow-up exam, additional tests and help navigating their care, Fendrick said.
“It makes no sense that the few people who actually benefit from free screening are the ones who have to pay to complete the screening process,” Fendrick said in an interview. “Basically, the issue is that everyone who tests negative gets to leave scot-free, unless and until they get a surprise bill for follow-up care.”
In an article for the Tradeoffs Podcast, reporter and producer Alex Olgin quoted Fendrick explaining that not requiring patients to pay for an initial screening test for colorectal cancer is cost-effective. “Because most people are negative, the math just works out in a way that if you waive cost sharing for follow up, it is actually made up by getting more people to get less expensive initial tests,” Fendrick told Olgin.
“Cheaper, reliable at-home screening tests don’t yet exist for lung, breast and cervical cancers,” Olgin added. “However, home tests are in development for human papillomavirus (HPV), the virus that causes cervical cancer.”
Resources
- “Recommendations From the Women’s Preventive Services Initiative on Breast Cancer Screening for Women at Average Risk and Patient Navigation Services for Breast and Cervical Cancer Screening,” Obstetrics & Gynecology, September 2025.
- “Evidence-Based Federal Policies Aim To Increase Cancer Screening Follow-Up, Though Barriers Remain,” Mark Fendrick, M.D., Michelle Moniz, M.D., and Kara Gavin, the V-BID Center, August 2025.
- “From Breast Cancer Screening to Diagnosis: New Recommendations for Expanded Coverage and Patient Navigation,” JAMA Internal Medicine, July 14, 2025.
- “Kennedy v. Braidwood: The Supreme Court Upheld ACA Preventive Services but That’s Not the End of the Story,” KFF, June 27, 2025.
- “Patient Navigation Services for Breast and Cervical Cancer Screening and Follow-Up: A Meta-Analysis,” JAMA Internal Medicine, June 9, 2025.
- “The unexpected costs of ‘free’ preventive care,” Bryn Nelson and William Faquin, M.D., Cancer Cytopathology, November 2023.
- “The Push to End Cancer Screening Purgatory,” Alex Olgin, Tradeoffs, Sept. 29, 2022.
- “Woman hit with nearly $2,000 unexpected bill for colon cancer screening,” Anna Werner, CBS News, June 29, 2021.
