A new program that Iowa Health and Human Services said will help people get better mental and behavioral health care in one place is being implemented, but with it comes the end of a program that thousands of Iowans say is much needed. According to the Iowa HHS website, on July 1, Iowa Medicaid began “sunsetting” the Integrated Health Home program. It was then announced that Iowa HHS is starting a new program called Certified Community Behavioral Health Clinics. KCCI reached out to Iowa HHS on Wednesday. No one could speak on camera Thursday, but a member of the department’s communications department did share a lot of information about the new program with KCCI via e-mail. According to the e-mail, Certified Community Behavioral Health clinics are designed to provide a range of mental health and substance use services. It is also stated that the clinics serve anyone who walk through the doors regardless of diagnosis or insurance status. Iowa HHS says IHH focused on care coordination for a “limited population of Medicaid enrollees with mental health diagnoses.”According to the Iowa HHS website, CCBHCs must meet certification criteria and must provide or coordinate nine core services, which include 24-hour mobile crisis teams, targeted case management, and outpatient mental health and substance use services. This end of the IHH program, however, has caused concerns for many people who are a part of it. “The biggest concern is for individuals that need help navigating the system with disabilities,” said Marie Christian, who has been helped through the program for several years. Christian said the program has been instrumental in her life. IHH provides her and thousands of other Iowans with a mental health disorder who are Medicaid members with a care coordinator. “That care coordinator goes out, gets to know them, does a very lengthy assessment to identify what their needs are,” said Mackenzi McIlhon, a habilitation program manager at Stepping Stone Family Services.Her title is one she says has recently changed. A week ago, it was “care coordinator” with the IHH program.“The care coordinator also works with that member to develop a treatment plan. We create goals. We identify what support and services we would likely be able to put in place. Then we just work with that member to figure out a way to best meet their needs and improve their overall well-being,” McIlhon said. It’s an important role and one that Christian and many others say they don’t know how they’d go on without it or the IHH program. “I struggle with brain fog and just remembering to do certain things. They’ve been the person that’s like, OK, here’s a reminder: this form is coming due, and they can assist with that,” said Christian, who also shared how her care coordinator helped her after she had a procedure. “He helped me get in touch to get some meal delivery things lined up. He helped me try to get connected with any resources that might be available.” For Jason Heckert, who says he has major depression, anxiety, panic disorder, and symptoms of agoraphobia, care coordinators like the one he works with have changed his life. “It’s life-changing. It saved my life on multiple occasions and not just through Sarah, but through the other workers that I’ve had over the years,” Heckert said. “They help bring me back to center so that I can progress, try to get back to work, and try to get back to being productive.” It’s for that reason and others that Heckert has spent time sending e-mails and reaching out to state leaders.It was noted in the e-mail from Iowa HHS that Iowa Medicaid has been actively discussing the future of IHH with providers and members for over a year. According to the communications department, there have been significant issues in the IHH program over the last several years, which caused a heavy administrative burden for providers to come into compliance with the required standards. Some issues listed in the e-mail from Iowa HHS to KCCI include a 2023 class-action lawsuit filed on behalf of Medicaid-eligible children “who had serious emotional disturbances, alleging ‘longstanding failure’ to provide legally required and medically necessary intensive home and community-based services.” Despite what comes with CCBHCs, there are people who worry that it won’t be as helpful to those who are enrolled in the IHH program. “We look at the whole person and not just their diagnosis,” McIlhon said. “Without that care and compassion — if that isn’t continued through these transitions — a lot of our members are really going to struggle.” “I just feel like I’m going to get lost in the shuffle and there’s going to be miscommunication,” Heckert said. “Like I said before, continuity and consistency is so important for people like me because we don’t have the control over our minds that we would through things like panic attacks.”
DES MOINES, Iowa —
A new program that Iowa Health and Human Services said will help people get better mental and behavioral health care in one place is being implemented, but with it comes the end of a program that thousands of Iowans say is much needed.
According to the Iowa HHS website, on July 1, Iowa Medicaid began “sunsetting” the Integrated Health Home program. It was then announced that Iowa HHS is starting a new program called Certified Community Behavioral Health Clinics.
KCCI reached out to Iowa HHS on Wednesday. No one could speak on camera Thursday, but a member of the department’s communications department did share a lot of information about the new program with KCCI via e-mail.
According to the e-mail, Certified Community Behavioral Health clinics are designed to provide a range of mental health and substance use services. It is also stated that the clinics serve anyone who walk through the doors regardless of diagnosis or insurance status. Iowa HHS says IHH focused on care coordination for a “limited population of Medicaid enrollees with mental health diagnoses.”
According to the Iowa HHS website, CCBHCs must meet certification criteria and must provide or coordinate nine core services, which include 24-hour mobile crisis teams, targeted case management, and outpatient mental health and substance use services.
This end of the IHH program, however, has caused concerns for many people who are a part of it.
“The biggest concern is for individuals that need help navigating the system with disabilities,” said Marie Christian, who has been helped through the program for several years.
Christian said the program has been instrumental in her life.
IHH provides her and thousands of other Iowans with a mental health disorder who are Medicaid members with a care coordinator.
“That care coordinator goes out, gets to know them, does a very lengthy assessment to identify what their needs are,” said Mackenzi McIlhon, a habilitation program manager at Stepping Stone Family Services.
Her title is one she says has recently changed. A week ago, it was “care coordinator” with the IHH program.
“The care coordinator also works with that member to develop a treatment plan. We create goals. We identify what support and services we would likely be able to put in place. Then we just work with that member to figure out a way to best meet their needs and improve their overall well-being,” McIlhon said.
It’s an important role and one that Christian and many others say they don’t know how they’d go on without it or the IHH program.
“I struggle with brain fog and just remembering to do certain things. They’ve been the person that’s like, OK, here’s a reminder: this form is coming due, and they can assist with that,” said Christian, who also shared how her care coordinator helped her after she had a procedure. “He helped me get in touch to get some meal delivery things lined up. He helped me try to get connected with any resources that might be available.”
For Jason Heckert, who says he has major depression, anxiety, panic disorder, and symptoms of agoraphobia, care coordinators like the one he works with have changed his life.
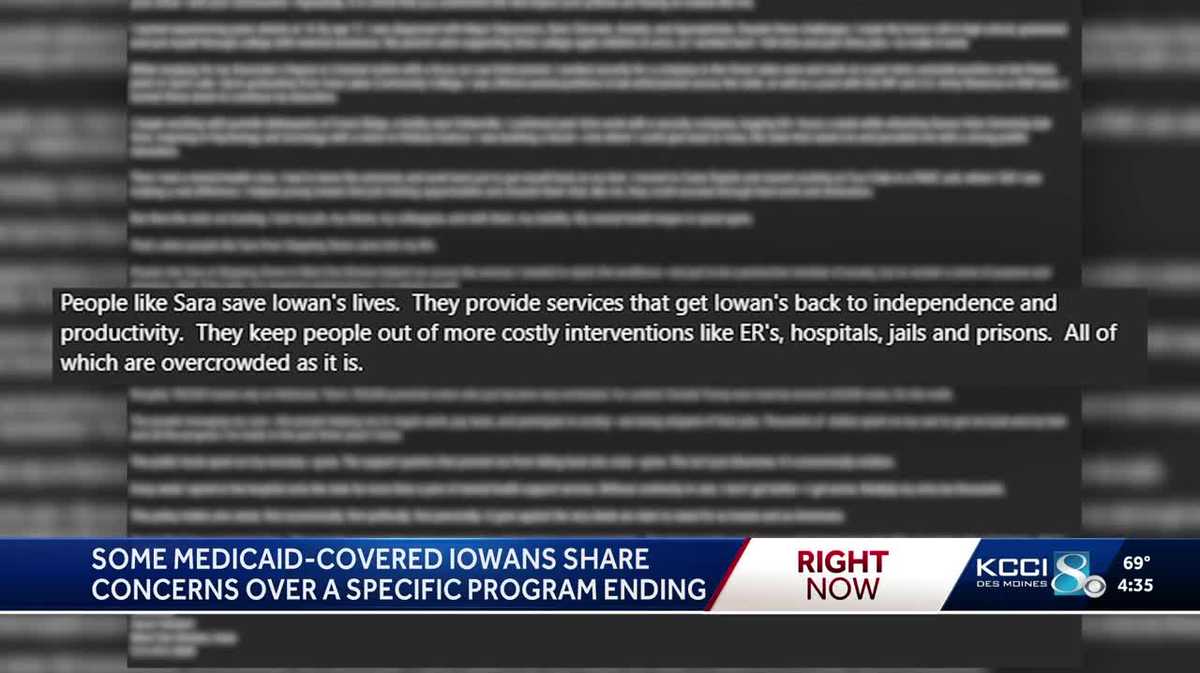
“It’s life-changing. It saved my life on multiple occasions and not just through Sarah, but through the other workers that I’ve had over the years,” Heckert said. “They help bring me back to center so that I can progress, try to get back to work, and try to get back to being productive.”
It’s for that reason and others that Heckert has spent time sending e-mails and reaching out to state leaders.
It was noted in the e-mail from Iowa HHS that Iowa Medicaid has been actively discussing the future of IHH with providers and members for over a year. According to the communications department, there have been significant issues in the IHH program over the last several years, which caused a heavy administrative burden for providers to come into compliance with the required standards.
Some issues listed in the e-mail from Iowa HHS to KCCI include a 2023 class-action lawsuit filed on behalf of Medicaid-eligible children “who had serious emotional disturbances, alleging ‘longstanding failure’ to provide legally required and medically necessary intensive home and community-based services.”
Despite what comes with CCBHCs, there are people who worry that it won’t be as helpful to those who are enrolled in the IHH program.
“We look at the whole person and not just their diagnosis,” McIlhon said. “Without that care and compassion — if that isn’t continued through these transitions — a lot of our members are really going to struggle.”
“I just feel like I’m going to get lost in the shuffle and there’s going to be miscommunication,” Heckert said. “Like I said before, continuity and consistency is so important for people like me because we don’t have the control over our minds that we would through things like panic attacks.”