By decoding the blood-brain barrier’s intricate structure and function, researchers are paving the way for new therapies that can safely breach the brain’s toughest defense.
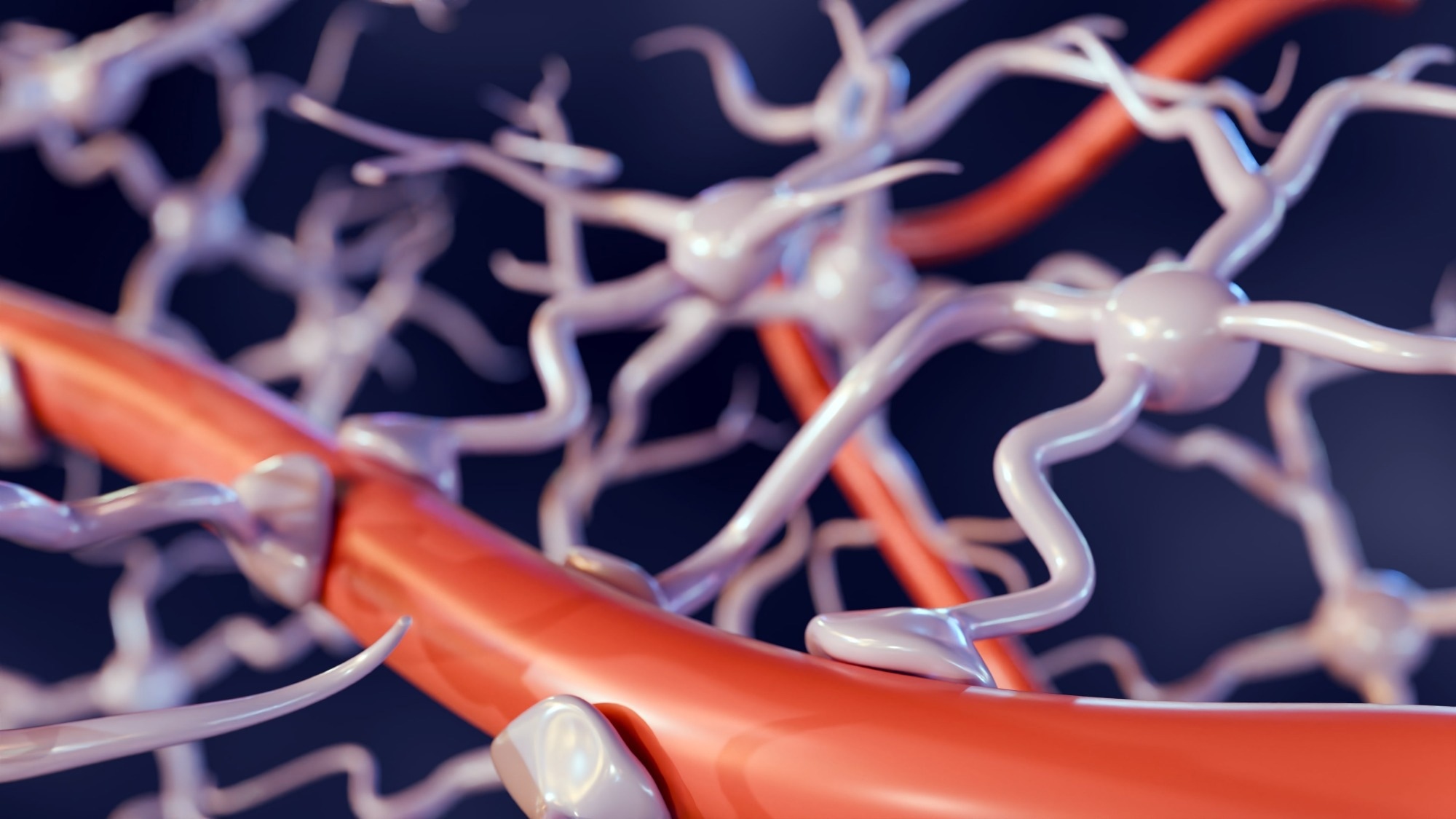
Primer: The blood–brain barrier. Image Credit: Love Employee / Shutterstock
In a recent primer paper published in the journal Current Biology, researchers elucidated the structure and function of the blood-brain barrier (BBB). It highlights the BBB as a complex, dynamic interface that separates the central nervous system (CNS) from general somatic blood circulation.
The primer also establishes how BBB dysfunction is a key feature in neurological diseases such as strokes and Alzheimer’s disease. It highlights additional mechanisms of barrier compromise in aging and cerebral small vessel disease, and future advances that may overcome the present limitations of neurological interventions hampered by BBB selectivity.
Background
Despite being the body’s command center, the brain is an incredibly delicate organ. While the skull provides physical protection against external trauma, internal threats from blood-borne toxins, pathogens, and activated immune cells require a different defensive approach, the blood-brain barrier (BBB).
First discovered in the late 19th and early 20th centuries, the BBB was conventionally perceived as an almost completely impermeable wall. However, pioneering work by Lina Stern and Raymond Gautier challenged this notion, demonstrating that the BBB could be crossed by certain substances and linking a substance’s cognitive effects to its ability to penetrate the BBB.
These findings shifted the scientific worldview from viewing the BBB as a wall to seeing it as an incredibly selective filter (now an established medical concept). Early comparative studies have since shown that BBB-like structures evolved independently in several animal lineages, from glial-based barriers in sharks to pericyte-free barriers in lampreys, underscoring evolutionary diversity.
The present primer paper addresses these knowledge gaps by elucidating the structural and functional benefits of the BBB.
The Structure of the Barrier
Decades of research on rodent models, other vertebrates, and humans have revealed that the mammalian BBB is a complex, multi-layered system, often called the neurogliovascular unit, comprising endothelial cells, pericytes, basement membranes, and astrocytes working in concert.
The unit is composed of three main types of cells that differ drastically in their structure and function:
Endothelial cells, which are ‘zippered’ together by proteins like claudin-5 and occludin, thereby forming a protective lining along the inner walls of the brain’s blood capillaries. These proteins have been observed to form tight junctions that drastically limit paracellular diffusion (leakage of substances between cells). A luminal endothelial glycocalyx, a proteoglycan-rich mesh, contributes to charge-selective exclusion and is an early casualty of BBB stress, presaging leukocyte infiltration.
Pericyte cells, known to support endothelial cell function by wrapping around the vessel and physically anchoring themselves via deep “peg-and-socket” invaginations. Pericytes are further revealed to function independently as critical regulators of barrier stability and integrity.
Astrocytes are a major type of brain glial (support) cell. High-resolution imaging of astrocytes has observed that these cells have processes (called “endfeet”) that ensheathe the brain’s vasculature. Endfeet are rich in aquaporin-4, a water channel that plays a pivotal role in regulating water homeostasis and clearing fluid to prevent edema (brain swelling), and in maintaining ion gradients through coordinated Na⁺/K⁺ exchange.
An important exception is the circumventricular organs, where fenestrated vessels permit freer exchange, buffered by deeper glia-immune barriers to maintain controlled CNS communication.
The Function of the Barrier
A substantial body of evidence has revealed that the BBB architecture creates a robust barrier to the entry of harmful elements while allowing the entry and exit of essential nutrients (required by the brain) and waste products (or signaling molecules), respectively. Selective transport has therefore been described as the primary function of the BBB, with vesicle-mediated transcytosis markedly repressed compared with peripheral endothelium.
Mechanistic investigations have demonstrated that transport through the BBB proceeds via several pathways:
Passive diffusion of small, lipophilic (fat-soluble) gases like oxygen (O₂) and carbon dioxide (CO₂) is known to occur readily across endothelial cell membranes.
Research has identified a “solute carrier superfamily” that facilitates transport and has been shown to provide dedicated BBB transport channels for essential nutrients. This includes the glucose transporter 1 (GLUT1), which promotes the absorption of over 100 grams of glucose (daily) to support the brain’s metabolic needs. Another, MFSD2A, transports docosahexaenoic acid (DHA), an omega-3 fatty acid critical for neuronal membranes. Other carriers, such as OATP/SLCO1A2, transport selected therapeutics and endogenous peptides across the BBB.
Active transport of large molecules, such as insulin or lipoproteins, has been observed to use receptor-mediated transcytosis. Specifically, these molecules bind to specific receptors on the cell surface, which then internalize the molecule in a vesicle and traffic it across the cell. Examples include LRP1, which traffics lipoprotein complexes and mediates amyloid-β clearance, and hormone receptors such as the insulin and leptin receptors.
“Efflux pumping,” refers to transporters that actively (using cellular energy) pump substances out of the brain. The best studied is P-glycoprotein (P-gp), which acts as a “bouncer,” using energy (in the form of ATP) to expel a wide range of xenobiotics (foreign substances) and metabolic waste.
Conclusions
The present primer paper elucidates the structure and function of the BBB, highlighting the dynamic filter’s role in housekeeping and the mechanisms it leverages to maintain physiological homeostasis. Unfortunately, it also reveals a limitation: the BBB’s effectiveness at blocking xenobiotics via efflux pumps like P-gp is a significant reason why many promising drugs for neurological disorders fail to reach their targets in the brain.
BBB impairment emerges early in aging and in APOE ε4 carriers and often co-occurs with cerebral small vessel disease, where chronic microvascular injury and pericyte loss degrade barrier integrity.
Systemic inflammatory states and infections such as COVID-19 can activate the endothelium, upregulate adhesion molecules, and transiently increase permeability, contributing to cognitive symptoms.
Encouragingly, future research is focused on developing patient-derived “organ-on-a-chip” models to better study the human BBB and designing nanotechnology-based delivery systems that can safely and precisely cross it. Mastering this barrier is key to treating the brain’s most challenging diseases.