Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, et al. American college of sports medicine roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. 2019;51(11):2391–402.
Kerr J, Anderson C, Lippman SM. Physical activity, sedentary behaviour, diet, and cancer: an update and emerging new evidence. Lancet Oncol. 2017;18(8):e457–71.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K. Body fatness and cancer—viewpoint of the IARC working group. N Engl J Med. 2016;375(8):794–8.
Koelwyn GJ, Quail DF, Zhang X, White RM, Jones LW. Exercise-dependent regulation of the tumour microenvironment. Nat Rev Cancer. 2017;17(10):620–32.
Hojman P, Gehl J, Christensen JF, Pedersen BK. Molecular mechanisms linking exercise to cancer prevention and treatment. Cell Metab. 2018;27(1):10–21.
Bouchard C, Ordovás J. Progress in molecular biology and translational science. San Diego: Academic Press; 2012.
Islami F, Marlow EC, Thomson B, McCullough ML, Rumgay H, Gapstur SM, et al. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019. CA Cancer J Clin. 2024. https://doi.org/10.3322/caac.21858.
Centers for Disease Control and Prevention. Obesity and cancer. Atlanta (GA): CDC; 2025. Available from: https://www.cdc.gov/cancer/risk-factors/obesity.html#:~:text=Obesity%2Dassociated%20cancers,the%20United%20States%20each%20year. Updated 2025 Jan 14; Cited 9 Sep 2025.
Feng X, Li R, Yi H, Chen S, Liu M, Wu Y. Global cancer burden attributable to excess body weight, 1990 to 2021, decomposed by population size, aging, and epidemiological change. Obesity. 2025;33(3):567–77.
Rock CL, Thomson C, Gansler T, Gapstur SM, McCullough ML, Patel AV, et al. American Cancer Society guideline for diet and physical activity for cancer prevention. CA Cancer J Clin. 2020;70(4):245–71.
World Cancer Research Fund/American Institute for Cancer Research. Continuous update project expert report 2018. Alcoholic drinks and the risk of cancer. London: WCRF International; 2018.
Taylor L. Third of adults are not getting enough physical activity, says WHO. BMJ. 2024; q1428.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020.
Chau JY, Merom D, Grunseit A, Rissel C, Bauman AE, van der Ploeg HP. Temporal trends in non-occupational sedentary behaviours from Australian time use surveys 1992, 1997 and 2006. Int J Behav Nutr Phys Act. 2012;9:76.
Ekelund U, Steene-Johannessen J, Brown WJ, Fagerland MW, Owen N, Powell KE, et al. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet. 2016;388(10051):1302–10.
Clinton SK, Giovannucci EL, Hursting SD. The world cancer research fund/American institute for cancer research third expert report on diet, nutrition, physical activity, and cancer: impact and future directions. J Nutr. 2020;150(4):663–71.
US Department of Health and Human Services. 2018 physical activity guidelines advisory committee scientific report. Washington (DC): USDHHS; 2018.
Matthews CE, Moore SC, Arem H, Cook MB, Trabert B, Håkansson N, et al. Amount and intensity of leisure-time physical activity and lower cancer risk. J Clin Oncol. 2020;38(7):686–97.
Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, et al. Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 million adults. JAMA Intern Med. 2016;176(6):816.
Guo F, McGee EE, Chiu YH, Giovannucci E, Mucci LA, Dickerman BA. Evaluating recommendation-based dietary and physical activity strategies for prostate cancer prevention: a target trial emulation in the health professionals follow-up study. Am J Epidemiol. 2024. https://doi.org/10.1093/aje/kwae184.
McGee EE, Hernán MA, Giovannucci E, Mucci LA, Chiu YH, Eliassen AH, et al. Estimating the effects of lifestyle interventions on mortality among cancer survivors: a methodological framework. Epidemiology. 2025.
Hernán MA, Robins JM. Using big data to emulate a target trial when a randomized trial is not available. Am J Epidemiol. 2016;183(8):758–64.
Dickerman BA, García-Albéniz X, Logan RW, Denaxas S, Hernán MA. Avoidable flaws in observational analyses: an application to statins and cancer. Nat Med. 2019;25(10):1601–6.
Thun MJ, Calle EE, Rodriguez C, Wingo PA. Epidemiological research at the American Cancer Society. Cancer Epidemiol Biomarkers Prev. 2000;9(9):861–8.
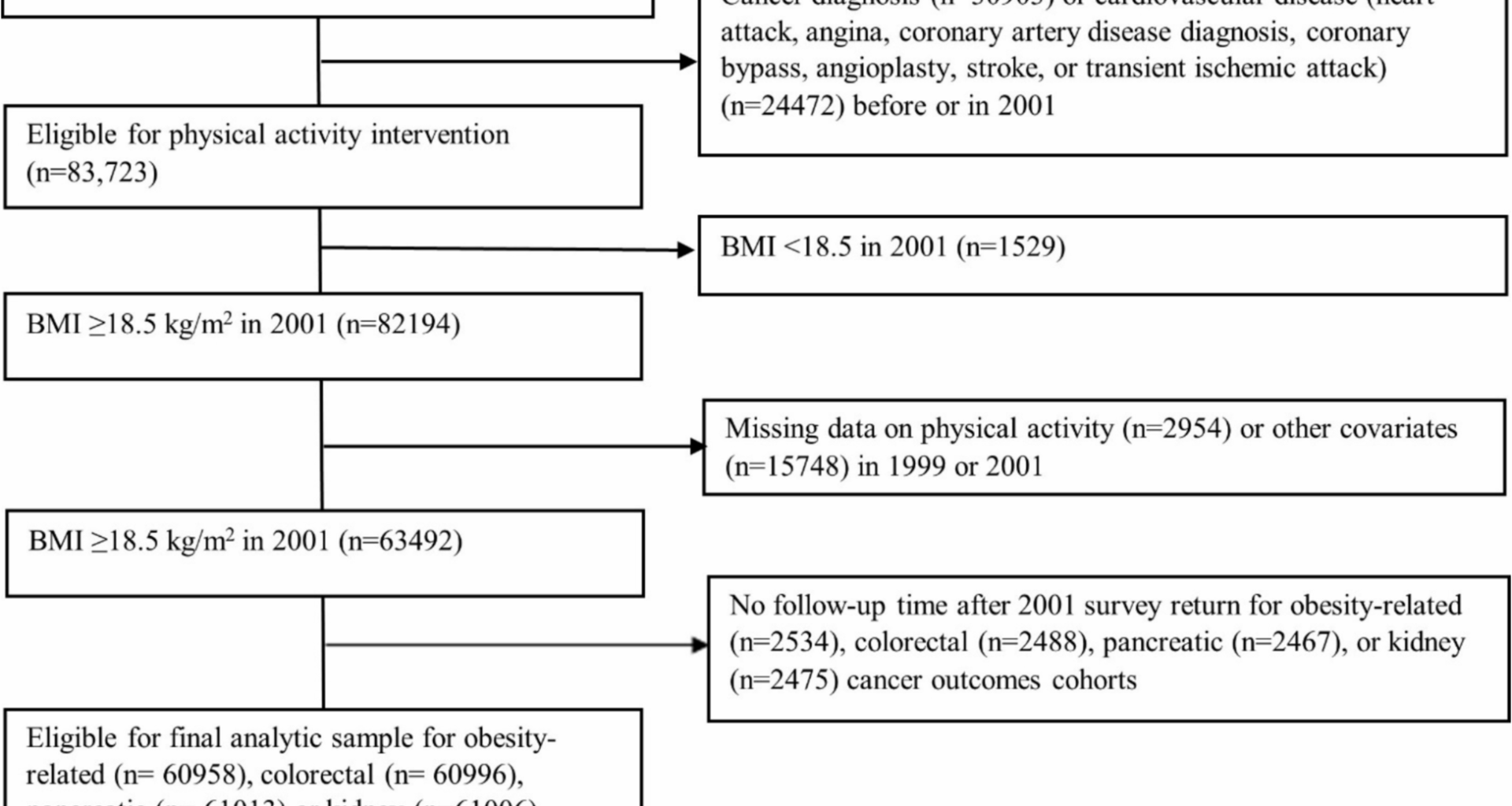
Calle EE, Rodriguez C, Jacobs EJ, Almon ML, Chao A, McCullough ML, et al. The American Cancer Society Cancer Prevention Study II Nutrition Cohort. Cancer. 2002;94(2):500–11.
McCullough ML, Patel AV, Kushi LH, Patel R, Willett WC, Doyle C, et al. Following cancer prevention guidelines reduces risk of cancer, cardiovascular disease, and all-cause mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(6):1089–97.
Calle EE, Terrell DD. Utility of the National Death Index for ascertainment of mortality among Cancer Prevention Study II participants. Am J Epidemiol. 1993;137(2):235–41.
Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23(5):991–9.
Rees-Punia E, Patel AV, Nocera JR, Chantaprasopsuk S, Demark-Wahnefried W, Leach CR, et al. Self-reported physical activity, sitting time, and mental and physical health among older cancer survivors compared with adults without a history of cancer. Cancer. 2021;127(1):115–23.
US Department of Health and Human Services. 2008 physical activity guidelines for Americans. Hyattsville (MD): USDHHS; 2008.
Young JG, Hernán MA, Robins JM. Identification, estimation and approximation of risk under interventions that depend on the natural value of treatment using observational data. Epidemiol Methods. 2014;3(1):1–19.
Hernán MA. IP weighting and marginal structural models. In: Hernán MA, Robins JM. Causal inference: what if. Boca Raton: Chapman & Hall/CRC; 2020.
Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. 2016;79:70–5.
Robins J. A new approach to causal inference in mortality studies with a sustained exposure period—application to control of the healthy worker survivor effect. Math Model. 1986;7(9–12):1393–512.
Taubman SL, Robins JM, Mittleman MA, Hernán MA. Intervening on risk factors for coronary heart disease: an application of the parametric g-formula. Int J Epidemiol. 2009;38(6):1599–611.
Robins J, Hernán M, Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G. Longitudinal data analysis. In: Fitzmaurice G, Davidian M, Verbeke G, Molenberghs G, editors. Handbooks of modern statistical methods. Boca Raton: Chapman & Hall/CRC; 2009. p. 553–99.
Loh WW, Ren D, West SG. Parametric g-formula for testing time-varying causal effects: what it is, why it matters, and how to implement it in Lavaan. Multivar Behav Res. 2024;59(5):995–1018.
Rudolph JE, Cartus A, Bodnar LM, Schisterman EF, Naimi AI. The role of the natural course in causal analysis. Am J Epidemiol. 2022;191(2):341–8.
Chiu YH, Wen L, McGrath S, Logan R, Dahabreh IJ, Hernán MA. Evaluating model specification when using the parametric g-formula in the presence of censoring. Am J Epidemiol. 2023;192(11):1887–95.
Young JG, Stensrud MJ, Tchetgen Tchetgen EJ, Hernán MA. A causal framework for classical statistical estimands in failure-time settings with competing events. Stat Med. 2020;39(8):1199–236.
Syriopoulou E, Mozumder SI, Rutherford MJ, Lambert PC. Estimating causal effects in the presence of competing events using regression standardisation with the Stata command standsurv. BMC Med Res Methodol. 2022;22(1):226.
Hernán MA, Robins JM. Causal inference: what if. Boca Raton: Chapman & Hall/CRC; 2020.
Sun M, Bjørge T, Teleka S, Engeland A, Wennberg P, Häggström C, et al. Interaction of leisure-time physical activity with body mass index on the risk of obesity-related cancers: a pooled study. Int J Cancer. 2022;151(6):859–68.
Danaei G, Robins JM, Hu FB, Manson JE, Hernán MA. Weight loss and coronary heart disease. Epidemiology. 2015:1.
Liu Y, Li Y, Bai YP, Fan XX. Association between physical activity and lower risk of lung cancer: a meta-analysis of cohort studies. Front Oncol. 2019. https://doi.org/10.3389/fonc.2019.00005.
Hernán MA, Hernández-Díaz S, Robins JM. A structural approach to selection bias. Epidemiology. 2004;15(5):615–25.
Sturgeon KM, Schweitzer A, Leonard JJ, Tobias DK, Liu Y, Cespedes Feliciano E, et al. Physical activity induced protection against breast cancer risk associated with delayed parity. Physiol Behav. 2017;169:52–8.
Raglan O, Kalliala I, Markozannes G, Cividini S, Gunter MJ, Nautiyal J, et al. Risk factors for endometrial cancer: an umbrella review of the literature. Int J Cancer. 2019;145(7):1719–30.
Sultana A, Rana S. Mechanisms underlying obesity-malignancy connection: a systematic narrative review. J Physiol Biochem. 2025. https://doi.org/10.1007/s13105-025-01084-9.
Onstad MA, Schmandt RE, Lu KH. Addressing the role of obesity in endometrial cancer risk, prevention, and treatment. J Clin Oncol. 2016;34(35):4225–30.
Patel AV. Obesity, recreational physical activity, and risk of pancreatic cancer in a large U.S. cohort. Cancer Epidemiol Biomarkers Prev. 2005;14(2):459–66.
Hildebrand JS, Gapstur SM, Campbell PT, Gaudet MM, Patel AV. Recreational physical activity and leisure-time sitting in relation to postmenopausal breast cancer risk. Cancer Epidemiol Biomarkers Prev. 2013;22(10):1906–12.
McTiernan A, Friedenreich CM, Katzmarzyk PT, Powell KE, Macko R, Buchner D, et al. Physical activity in cancer prevention and survival: a systematic review. Med Sci Sports Exerc. 2019;51(6):1252–61.
Warner ET, Wolin KY, Duncan DT, Heil DP, Askew S, Bennett GG. Differential accuracy of physical activity self-report by body mass index. Am J Health Behav. 2012;36(2):168–78.
Ashtary-Larky D, Lamuchi-Deli N, Milajerdi A, Salehi MB, Alipour M, Kooti W, et al. Inflammatory and biochemical biomarkers in response to high intensity resistance training in trained and untrained men. Asian J Sports Med. 2017;8(2).
Weiss EP, Royer NK, Fisher JS, Holloszy JO, Fontana L. Postprandial plasma incretin hormones in exercise-trained versus untrained subjects. Med Sci Sports Exerc. 2014;46(6):1098–103.
Holten MK, Zacho M, Gaster M, Juel C, Wojtaszewski JFP, Dela F. Strength training increases insulin-mediated glucose uptake, GLUT4 content, and insulin signaling in skeletal muscle in patients with type 2 diabetes. Diabetes. 2004;53(2):294–305.
Bloom SR, Johnson RH, Park DM, Rennie MJ, Sulaiman WR. Differences in the metabolic and hormonal response to exercise between racing cyclists and untrained individuals. J Physiol. 1976;258(1):1–18.
Fukuoka Y, Haskell W, Vittinghoff E. New insights into discrepancies between self-reported and accelerometer-measured moderate to vigorous physical activity among women—the mPED trial. BMC Public Health. 2016. https://doi.org/10.1186/s12889-016-3348-7.
Hernán MA. The hazards of hazard ratios. Epidemiology. 2010;21(1):13–5.
Chiu YH, Stensrud MJ, Dahabreh IJ, Rinaudo P, Diamond MP, Hsu J, et al. The effect of prenatal treatments on offspring events in the presence of competing events. Epidemiology. 2020;31(5):636–43.
Chlebowski RT, Anderson GL, Aragaki AK, Manson JE, Stefanick ML, Pan K, et al. Association of menopausal hormone therapy with breast cancer incidence and mortality during long-term follow-up of the Women’s Health Initiative randomized clinical trials. JAMA. 2020;324(4):369.
Dib BN, Swanson SA. Emulating a target trial using observational data. JAMA Intern Med. 2025;185(4):459–60.
Cole SR, Hernán MA. Constructing inverse probability weights for marginal structural models. Am J Epidemiol. 2008;168(6):656–64.
Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–8.