Our study revealed that 62.9% of community pharmacists exhibited a high level of knowledge regarding MTM services. This proportion is notably higher than the reported levels in Kenya23 and Lebanon26 yet remains substantially lower than those observed in Nigeria (94%)27, Indonesia (74.9%)25, and Malaysia (97.5%)28. These discrepancies may be due to differences in practice settings, exposure to patient-centered care, and access to MTM training. For instance, hospital pharmacists are more exposed to inter-professional collaboration and clinical practices than those in community settings. Furthermore, access to continuing professional development and structured educational programs varies widely across countries, which may contribute to these observed knowledge gaps20. This emphasizes the need to strengthen MTM-focused continued professional development opportunities within community pharmacies, particularly in resource-limited settings.
While most pharmacists recognized the beneficiaries and role of MTM in assisting with medication adherence and disease control—a finding consistent with earlier studies21,28, a large majority lacked an understanding of the core elements and goals of MTM. This is in contrasts to studies conducted in Jordan, Yemen, and Malaysia, where most pharmacists correctly identified the goals and core elements of MTM21,22,28. Due to their accessibility and drug therapy knowledge, pharmacists are well-positioned to serve as valuable providers of MTM services2. Therefore, to bridge the knowledge gap and ensure effective service delivery, it is essential for pharmacy professionals to receive adequate training on the goals, core elements, and overall benefits of MTM. Moreover, similar to the findings from Jordan and Yemen21,22, our study found that younger pharmacy professionals had a higher level of MTM knowledge. This could be due to a shift in pharmacy education and practice with young pharmacists thought to provide patient-centered care, such as MTM12.
With respect to attitude, only 45.7% of participants in our study exhibited a positive attitude toward MTM, a figure considerably lower than those reported in Jordan, Yemen, Nigeria, Malaysia, and Saudi Arabia21,22,27,28,29. Notably, less than half of the respondents supported the core elements of MTM and viewed it as a unique opportunity for pharmacists to participate in patient care on a broader scale. This finding diverges from reports in Yemen, Jordan, and the United States21,22,30, where the majority of pharmacists supported both the core elements and the impact of MTM services in patient care. For example, in the United States, over 90.1% and 86.2% of pharmacists agreed that MTM services are a valuable service that enhance pharmacy practice career, and supports higher levels of patient care. Such discrepancies may stem from differences in healthcare delivery systems, workplace expectations, and availability of MTM-specific training. In settings where dispensing is prioritized over clinical services, pharmacists may view MTM as an added burden rather than a valuable service. Similar to previous studies25,27, our findings also showed that gender and level of qualification are associated with attitudes towards MTM, indicating demographic and educational factors may further influence pharmacy professionals’ perceptions of MTM services.
In the current study, only 41.9% of participants demonstrated good MTM practices, This proportion is higher than those reported in Yemen (11% ) and the USA (10%)22,31 but lower than rates observed in Indonesia (57.9%)25 and two studies from Nigeria24,27. Among the MTM services, verbal education and training was the most frequently performed activity. However, consistent with previous studies21,22,25,32, more advanced practices—such as formulating a medication treatment plan, performing a comprehensive medication review, documenting the care provided, and monitoring and evaluating the patient’s response to therapy, were seldom practiced. This limited engagement may be due to a lack of skills in managing patient compliance and review therapy33. Encouragingly, evidence indicates that most pharmacists would be willing to provide MTM if they received appropriate training34, which supports the need to enhance training and continued professional development initiatives. Targeted training as well as systematic integration of MTM processes supported by comprehensive training for both pharmacists and pharmacy technicians enables to tailor MTM to routine workflows, increase MTM completion rates and leads to marked improvement in comprehensive medication review35,36. Combined with supportive policies that establish clear pharmacists’ roles and reimbursements37, these interventions can ensure effective and sustainable MTM services in community pharmacies. Similar to findings from other studies25,38, our study showed that pharmacy professionals with ten or fewer years of practice were more likely to demonstrate good MTM practices. This might be due to greater confidence in those with fewer years of practices, who are more familiar with patient-centered care32.
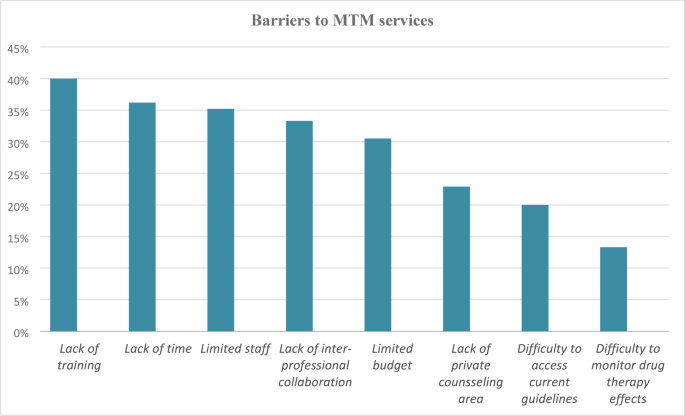
Similar to findings widely reported in the literature, the most common barriers to delivering MTM services in this study were lack of training, lack of time, limited staff, and lack of inter-professional collaboration. A recent systematic review comprehensively highlighted these barriers across diverse healthcare settings, underscoring the impact on effective implementation of MTM20. Consistent with our findings, previous studies have also revealed similar constraints in MTM service delivery21,25,26,27,28,39. Lack of training has consistently emerged as a significant barrier, impeding pharmacists’ confidence and competence in delivering MTM16,39. Moreover, a lack of training may intensify other challenges such as time management within busy pharmacy workflows and collaboration with other healthcare providers21,25. Therefore, addressing training gaps through structured educational programs is recommended to enhance pharmacists’ skills and self-efficacy, which may indirectly allow them to overcome other barriers such as time management, inter-professional relationships, and staffing pressure by improving efficient work flow and prioritization of MTM services34,35,36.
Limitations: This is a cross-sectional study design with a small sample size, which may restrict the generalizability of the findings to all community pharmacy professionals in Ethiopia. Consequently, future studies should consider a nationwide study with a large sample size to provide more representative data. Moreover, interventional studies aimed at designing an educational intervention to improve pharmacy professionals’ attitudes and practices toward MTM are needed. Despite these limitations, this is the first study in Ethiopia to explore community pharmacy professionals’ KAP regarding MTM, providing a baseline for future researches and policy development.