Crystal Mackall: There are numerous bottlenecks. First, manufacturing of autologous products requires complex logistics wherein the product moves through a chain of custody from the collection site to the manufacturing site, then back to the administering site, with often two stops in the hospital before it makes it to the patient’s bedside. Point-of-care manufacturing or decentralized manufacturing could simplify and reduce the costs of the logistics associated with current autologous product manufacturing.
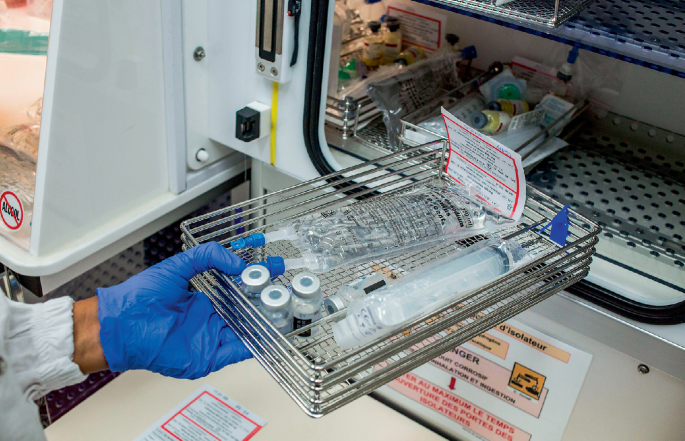
Second, products undergo a manufacturing process that is at a minimum three days and sometimes a couple of weeks, depending on the product. That process involves numerous reagents and procedures that render it expensive and results in often highly variable products. Autologous products will also be highly variable due to individual differences in clinical history, genotype, exposure etc. Automation provides an opportunity to drastically reduce the complexity and cost of the manufacturing process itself.
Third, quality control assays required by regulatory authorities are bespoke, complex, expensive and relatively non-standardized. Quality control analysis of individual products typically occurs outside of the workflow of manufacturing, adding complexity, cost and time. Integrating quality control in real time during product manufacturing would reduce costs and enhance product quality and enable economies. As an example, although many manufacturing processes have reduced the duration of cell culture from 10–14 days to 4–6 days, the amount of time it takes to release products to the patient hasn‘t changed substantially because additional time is needed to complete the quality control assays.
Fourth, viral vectors are expensive to produce and require very expensive quality control, and there remains a relative shortage of qualified manufacturers, leading to high costs and long wait times. The field hoped that this bottleneck could be overcome by using virus-free manufacturing that delivers nucleic acids directly into the cells. However, the field has witnessed high costs of DNA, plasmids, guide RNAs and critical reagents for virus-free manufacturing, resulting in essentially no cost reductions and continued challenges with long wait times to receive good manufacturing practice (GMP)-grade reagents. Increased competition in this space should decrease cost and increase availability, but we haven’t yet observed this. The United States and other developed countries should incentivize expanding the workforce and building state-of-the-art manufacturing for cell and gene therapies.
Rayne H. Rouce: One of the unique challenges related to manufacturing cell therapy products is that most of these products are autologous, manufactured directly from the patient. Thus, the quality and quantity of the starting products vary and are often influenced by prior treatments and/or underlying disease. Despite identical manufacturing processes, the resultant products can have different phenotypic and functional characteristics, which can affect outcomes. Due to the personalized nature of these products, associated costs and often fleeting window of opportunity for collection and manufacture, there is limited opportunity to manufacture a suitable product that meets all release criteria.
Additionally, the inherent complexities of cell therapies (particularly those that are gene-modified) require specialized reagents, specially trained personnel, clean-room infrastructure, and scalability. These have historically limited manufacture capabilities to large academic institutions or pharmaceutical companies in high-income countries. Fortunately, researchers and pharmaceutical and biotechnology companies are working toward solutions to address these bottlenecks in efforts to enhance access. Immediately available ‘off-the-shelf’ cell therapies incorporating built-in risk mitigation functionality, decentralized point-of-care manufacture using automated techniques that negate the requirement for specialized personnel and shorten release testing, and innovative approaches to scalability have been explored, with promising results.
Michael S. Pepper: From a lower-to-middle income (LMIC) country perspective (South Africa is a middle-income country), key bottlenecks include lack of funding, lack of capacity (know-how and infrastructure), an inadequate regulatory environment, and limited patient and public understanding. Central to the success of initiatives to overcome these challenges is a need for sensitivity and understanding of the local environment. Attempts to copy-and-paste from well-resourced settings have a lower likelihood of succeeding than those in which highly inclusive participation of local experts is a prerequisite. Funding should be linked to milestones and outputs. Capacity development must focus on upskilling demographically representative individuals. Overcoming regulatory hurdles requires the development in parallel of two workstreams: the first involves an understanding of existing legislation and how this might be linked to international best practice to meet short-term needs; the second involves the explicit and intentional drafting of legislation that will accommodate rapidly advancing technologies, both current and future. More generally, the lack of patient understanding stems not only from lack of exposure, but also from cultural and religious beliefs, as well as misinformation. A deep understanding of the local population from these perspectives is required for successful uptake.