Attempts to resuscitate Carol Taylor were so inept that a coroner issued a prevention of future deaths report
A widower whose wife died after attempts to resuscitate her failed, has called on a public inquiry to order urgent training of all NHS mental health staff.
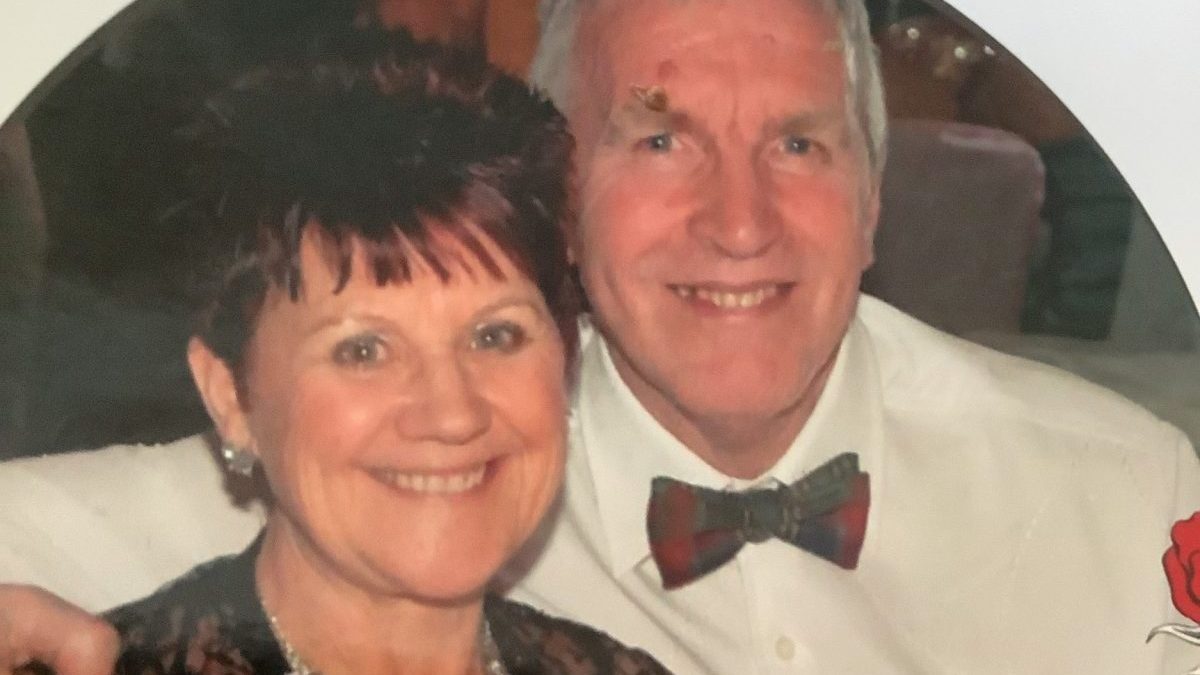
Former teacher Carol Taylor, 75, died of a pulmonary embolism while in the care of Essex Partnership University NHS Foundation Trust (EPUT), but attempts to resuscitate her were so inept that a coroner issued a prevention of future deaths report (PFD).
An inquest last month heard how staff at St Margaret’s Hospital in Essex had little idea of how to resuscitate her and even failed to turn an oxygen unit on.
Carol’s husband Ralph, 79, from Buckhurst Hill, Essex, who is a core participant at the Lampard Inquiry into mental health services, told The i Paper the EPUT’s failure to ensure staff were properly trained was “unforgiveable”.
Left traumatised
He said: “After Carol’s death my family were traumatised to learn of chaotic attempts to resuscitate her for which staff either failed to follow training or were inadequately trained. Subsequently I have learnt that similar concerns about resuscitation have been raised in previous inquests and the same mistakes have been repeated.
“This is unforgivable and encapsulates why affected families have completely lost confidence in EPUT’s ability to be involved in effecting the real changes required in mental health treatment. It is crucial that the Lampard Inquiry immediately addresses this issue and orders mental health staff be properly trained in basic lifesaving skills.”
At Carol’s inquest, coroner Stephen Simblet KC concluded the former primary school teacher died from natural causes but also issued a PFD which said: “There is no system that prevents staff that are non-compliant with mandatory training, including basic life support training, from being able to work on EPUT in-patient wards.
“This is a particular concern generally, but especially in hospitals such as St Margaret’s where at least some of the wards specialise in treating elderly patients who are likely to be at greater risk of medical collapse than the general population.”
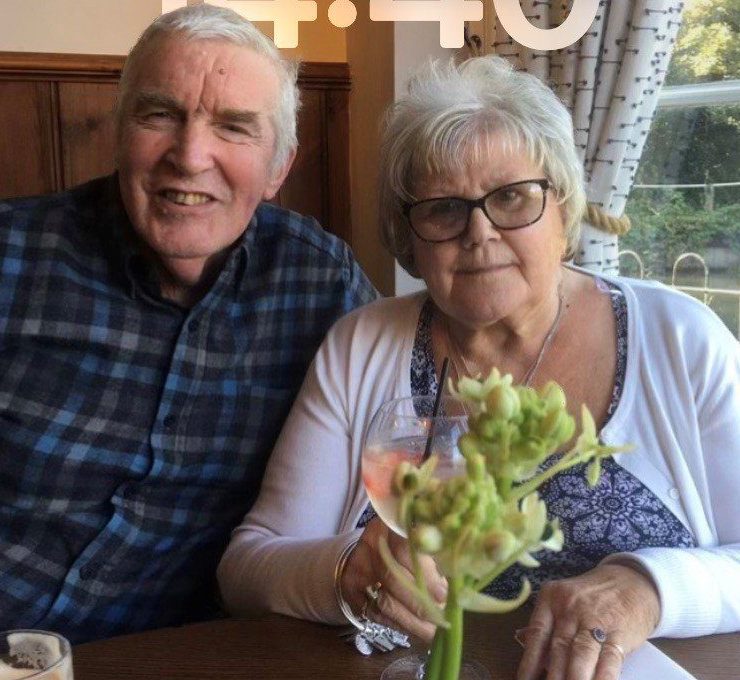 Not all of the staff on duty on the night Carol died were up to date with their mandatory CPR training, the inquest into her death found
Not all of the staff on duty on the night Carol died were up to date with their mandatory CPR training, the inquest into her death found
Carol was first treated for depression in December 2012 and discharged in April 2013, following which time Ralph described his wife’s condition as stable.
“Carol was very artistic and particularly enjoyed pottery and jewellery making as well as other crafts. She was also able to enjoy positive relationships with our five grandchildren, particularly the three granddaughters who live locally,” Ralph said.
“However, unfortunately she had a series of joint operations from 2010 to 2017 which progressively decreased her mobility and gave rise to associated debilitating physical conditions.”
The couple had not travelled abroad since 2011, but decided to go on a cruise in March 2023 to see the Northern lights to mark Carol’s forthcoming 75th birthday. Unfortunately, it proved disastrous as Carol developed pneumonia and had to be taken off the ship at Reykjavik, Iceland.
She was initially in hospital for a couple of weeks and then the couple stayed in a “hospital/hotel until we could be repatriated”, Ralph said.
Deteriorating mental health
While in Iceland Carol’s mental health deteriorated but on her return, despite her existing diagnosis, she was unable to get immediate psychiatric treatment.
Following an attempt to take her own life at the end of June 2023, she was transferred to St Margaret’s Hospital Epping in early July where she remained until her death on 21 November that year.
“Unfortunately, what happened that night was sadly shambolic,” Ralph said.
“After Carol was found unresponsive in her room, one of the staff was deputed to call the emergency services but didn’t know that in order to obtain an outside line they first had to dial 9 before 999.
“Although there were two staff members who attempted resuscitation, neither took the lead as I understand they are instructed to do.”
Two ambulances of paramedics responded to the call. The first arrived within the target time but were unfamiliar with the surroundings and there was no member of staff available to guide them into what is a secure unit.
When the first crew arrived in Carol’s room they found resuscitation was being carried out by staff with Carol on her side and not on her back as she should have been. The oxygen cylinder they were using was also not switched on.
Ralph said: “The first crew of paramedics took over the resuscitation from the staff and one of them asked the staff for details of Carol’s medical history which none of them were able to provide.
“Another crew of paramedics arrived and assisted the first crew. A member of the second crew who was experienced initiated a complaint about the mistakes being made in resuscitation by the staff.”
At the inquest it was determined that not all of the staff on duty on the night Carol died were up to date with their mandatory CPR training.
‘Shambolic and an utter disgrace’
Carol’s death follows a number of similar deaths of mental health patients in Essex where resuscitation was an issue, including in the case of teenager Elise Sebastian who died in EPUT care in 2021. In May, a jury inquest found neglect at her mental health unit contributed to the death of the “happy and outgoing” 16-year-old.
Priya Singh, partner at Hodge Jones & Allen which represents more than 120 victims and families at the Lampard Inquiry, including Ralph, said: “The attempts to resuscitate Carol were an absolute shambles and an utter disgrace. It is blatantly obvious from evidence that there were critical failings in the staff’s resuscitation attempts, indeed they were noted to be doing chest compressions to the patient whilst she was lying on her side.
“We see these issues around failures in resuscitation raised time and time again yet nothing is done. [Inquiry Chair] Baroness Lampard needs to make urgent recommendations to ensure mental health staff are trained so they can save the lives of patients in their care.”
Trust officials said resuscitation training has been enhanced – all registered staff working within an inpatient setting are now required to complete Resuscitation Council UK Immediate Life Support training which builds on the skills of basic life support to give staff the skills, knowledge and confidence to lead as first responders in an emergency situation. It said dedicated staff on each ward have also been appointed as Resuscitation Link Practitioners and play a key role in strengthening any response to emergency situations.
EPUT Chief Executive Paul Scott said: “My thoughts are with Carol’s family and loved ones and I send my condolences both personally and on behalf of the Trust.
“As the Inquiry progresses there will be many accounts of people who were much loved and missed over the past 24 years and I want to say how sorry I am for their loss. All of us across healthcare have a responsibility to work together to improve care and treatment for all and to build on the improvements that have already been made over the last 24 years.”
The Lampard Inquiry is the first public inquiry to specifically examine mental health deaths in the UK. It was granted following years of tireless campaigning by grieving families whose loved ones died while under the care of the Essex Partnership University Foundation NHS Trust (EPUT) and the North East London Foundation Trust (NELFT). The statutory inquiry is looking into more than 2,000 deaths of mental health inpatients in Essex between 2000 and 2023.
A spokesperson for the Inquiry said: “While the Inquiry can’t comment on individual cases, we recognise the loss that Ralph and his family have experienced, and extend our sympathy to them.
“The Chair has previously indicated that, where appropriate, she would consider making interim recommendations.
“However, the Inquiry cannot comment on potential recommendations while the investigation is ongoing. The final report and recommendations are currently expected to be published by the end of 2027.”
The next set of hearings will take place between 13 and 30 October at Arundel House, in London. The Inquiry is expected to make a number of recommendations to improve NHS mental health services across England.